An integrative perspective on influenza virus host interactions
Introduction of influenza virus
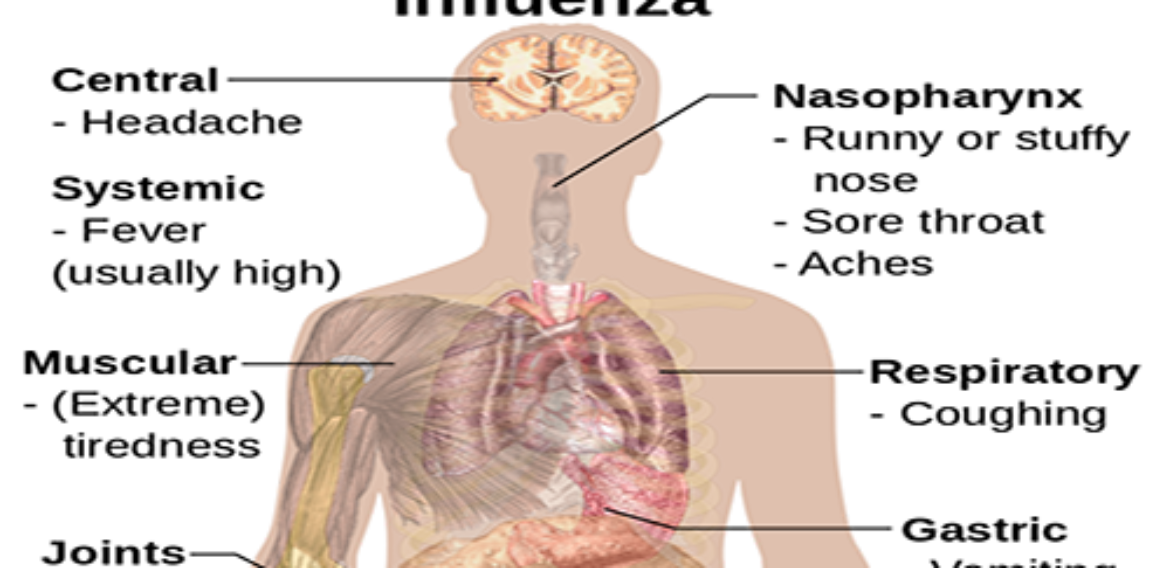
The epidemiologically important influenza viruses are negative-sense, enveloped, single-stranded RNA viruses that belong to the family Orthomyxoviridae (Palese & Shaw, 2006). These viruses infect about 5 to 15% of the world’s population annually, and they cause occasional pandemics with high rates of infection and death (WHO, 2003; Subbarao et al., 2006). Influenza virus infection results in a complex array of virus-host interactions, occurring across levels of biological organization, from cells to populations. These different levels of virus-host interactions have important consequences for influenza virus evolution and epidemiology. For example, cellular-level interactions determine the rate at which phenotypically consequential genetic variation is generated during infection, thereby influencing the tempo of influenza virus evolution. Organismal-level selection acts on the variation generated at the cellular level, increasing the relative frequencies of viruses that are least recognizable to the immune system. Subsequently, population-level herd immunity and other stochastic forces determine which products of the organismal-level selection will be responsible for influenza epidemics. In the following, we review important aspects of the cellular-, organismal-, and population-level interactions between influenza viruses and their human hosts, and discuss some of the gaps in our understanding of those interactions. We begin by describing the structural and genomic organization of influenza viruses, and conclude by discussing some open problems pertaining to influenza virus surveillance that could be addressed through an integrative study of the different levels of influenza virus-host interactions.
Genomic and structural organization of influenza viruses
There are three “types” of influenza viruses: A, B and C. These viruses have segmented genomes made up of RNA; the genomes of types A and B viruses contain 8 segments, while those of type C viruses contain 7 segments (Palese & Shaw, 2006; see Figure 1). The 8 segments of influenza A viruses code for a total of 11 proteins. Among these are the three proteins (named PA, PB1, and PB2) that make up the RNA-dependent RNA polymerase, which is responsible for viral transcription and replication. Each genomic segment is packaged into a viral ribonucleoprotein (vRNP) complex, comprising both NP and the RNA polymerase (Noda et al., 2006). The vRNPs are connected to the viral envelope by the M1 protein, which interacts directly with both HA, NA, and also with lipid molecules found in the envelope.
The HA and NA proteins form spikes that protrude into the exterior of the viral envelope (Fujiyoshi, 1994). In its native form, HA consists of a complex of three dimers, each of which contains a molecule of HA1 protein and a molecule of HA2 protein. HA1 and NA are the main targets of antibodies produced during infection. Differences in the reactivities of HA1 and NA with such antibodies form the bases for the classification of influenza A viruses into subtypes. Each subtype is denoted by a specific combination of HA and NA proteins that are markedly different with respect to their reactivity with antibodies. Finally, the M2 protein forms an ion channel that is critical to productive viral infection (Pinto et al., 1992), as we discuss later.
A cellular-level perspective on influenza-virus host interactions Entry into host cells
Human influenza viruses normally infect epithelial cells found in the respiratory tract. The viral HA attaches to membrane receptors found on the target cell surface, through electrostatic interactions (Flint et al., 2004). Following this attachment, the virus is internalized into the cell by endocytosis and trafficked through endosomal vesicles. As the endosomal pH drops to ~5.5, the M2 ion channel opens, allowing the influx of hydrogen ions into the interior of the viral particle (Pinto et al., 1992). The resulting decrease in pH causes vRNPs to be detached from the surrounding M1 protein. In addition, HA undergoes a conformational switch into a coiled coil of alpha helices, in which the HA2 subunit is reoriented towards the exterior of the molecule (Whittaker & Digard, 2006). HA2 subsequently mediates fusion of the viral envelope and the endosomal membrane, releasing vRNPs into the cytoplasm. These vRNPs are targeted to the nucleus by nuclear localization signals located on each of the three polymerase proteins as well as on NP. The details of this process are yet to be elucidated, although various components of the nuclear import machinery are likely to play an important role (Whittaker & Digard, 2006). Note that the activity of M2 is the target of some antiinfluenza virus drugs, such as amantadine (Gubareva & Hayden, 2006).
Transcription and replication of the viral genome
In the nucleus, the viral RNA (vRNA) is transcribed and subsequently replicated. The viral RNA-dependent RNA polymerase binds to a conserved sequence found in the 5′ end of the vRNA, and transcribes the bound vRNA. Transcribed viral mRNAs are exported to the cytoplasm where they are translated. The resulting proteins are targeted to the apical surface of the plasma membrane, where they are eventually packaged into progeny virions. Prior to its transport to the plasma membrane, newly synthesized HA (also called HA0) is cleaved to form HA1 and HA2 (Palese and Shaw, 2006). HA1 and HA2 combine to form a heterodimer, HA1-HA2, at the base of which is embedded the hydrophobic HA2. Subsequent trimerization of HA1-HA2 complexes yields the native form of HA. Note that mRNAs of the M and NS segments are spliced into two mRNAs that are respectively translated into M1 and M2 (in the case of the M segment) and NS1 and NS2 (in the case of the NS segment).
After a few rounds of transcription, the vRNA is replicated; first, the polymerase produces a complementary copy of the vRNA, the cRNA, which is encapsidated by NP. The cRNA is then copied back into vRNA. It is not yet clear what determines the =\”switch” to cRNA synthesis (and hence vRNA replication), or whether such a switch actually exists. Recent experimental evidence (Vreede et al., 2004; Vreede & Brownlee, 2007) suggest that both transcription and replication of the vRNA occur early during the infection process, and that the cRNA cannot be detected at this time because it is degraded by RNases found in the nucleus. According to this view, only after sufficient amounts of NP and the polymerase proteins have accumulated in the nucleus is the cRNA stabilized. Newly synthesized vRNA is packaged into vRNP and exported into the cytoplasm. Not much is known about the export process but the current hypothesis (Whittaker & Digard, 2006) holds that a few hours after the start of virus replication, newly synthesized M1 and NS2 enter the nucleus, where each molecule of M1 binds to a single molecule of vRNP and abrogates transcription and replication of that vRNP. NS2 then binds to the M1-vRNP complex and mediates export of the complex by means of its nuclear export signal.
Budding from infected host cells
The packaging of newly synthesized viral proteins into progeny virions is not well understood. The most plausible model of this process posits that each viral segment contains packaging signals that direct its specific incorporation into nascent virions. Such signals have been identified in the 5′ and 3′ terminal sequences of NA and other segments (Fujii et al., 2003; Marsh et al., 2008). An intriguing observation that lends further support to this model is the observation that defective NS2 segments are able to direct the selective incorporation of other defective segments into progeny virions (Odagiri & Tashiro, 1997). Following packaging, progeny virions bud through the plasma membrane and bind to the cell surface through interactions between HA and cell-surface receptors. The virions remain bound to the cell surface until these receptors are cleaved by NA. This activity of NA is the target of a class of anti-viral drugs called NA inhibitors (Gubareva & Hayden, 2006).
From a cellular- to an organismal-level perspective
The innate immune response to influenza virus infection
The innate immune system is the principal mode of host defense against primary influenza virus infection1. An important mediator of the innate immune response to viral infection is interferon (IFN, Ludwig et al., 2006). The mechanisms by which IFN combats viral infection at the cellular level are reviewed here. Connections between IFN and other cytokines produced by the innate immune response and the organismal-level, adaptive response are discussed in the next section. During infection, the cellular protein PKR encounters viral double-stranded RNA (dsRNA) and other products of viral replication, thereby becoming activated (Ludwig et al., 2006). Activated PKR phosphorylates the kinase IKKβ, and IKKβ in turn phosphorylates i-κB, which normally inhibits NF-κB transcription factors (Ludwig et al., 2006). Phosphorylated i-κB is subsequently degraded, thereby releasing NF-κB transcription factors. These transcription factors are translocated to the nucleus, where, together with other transcription factors, they induce the expression of type 1 IFNs, namely IFNα (of which there are many subtypes) and IFNβ. The IFNs are synthesized and secreted into the extracellular medium, where they induce neighboring cells to produce a variety of proteins that have both direct and indirect virus replication-inhibiting activities.
Specifically, IFN binds to its cell surface receptor, thereby activating two kinases, which in turn phosphorylate the transcription factors, STAT1 and STAT2 (Garcia-Sastre, 2001). Subsequently, STAT1 and STAT2 form a heterodimer and are translocated to the nucleus, where they bind to another transcription factor (called IFN regulatory factor 9) to form the heterotrimer, ISGF3. ISGF3 induces the transcription of up to 300 genes, including the genes that code for PKR, the 2-5A synthetases, and the Mx proteins. PKR further induces the expression of IFN, resulting in a positive feedback loop linking IFN induction to PKR production (Garcia-Sastre, 2001). The 2-5A synthetases become activated upon encounter with dsRNA and subsequently activate a latent RNase, which degrades viral mRNAs, thereby decreasing the amount of viral proteins synthesized. The Mx proteins inhibit viral replication by interacting directly with the PB2 and NP proteins (Turan et al., 2004). Furthermore, PKR mediates phosphorylation of the important translation initiation factor, eIF-2α, thereby abrogating the synthesis of viral proteins (Garcia-Sastre, 2001).
Influenza viruses also activate a variety of signaling pathways, such as the ERK, p38, ERK5, and JNK pathways (Ludwig et al., 2006). The downstream components of some of these pathways (e.g., the ERK5 pathway) are not known. The ERK and JNK pathways are believed to induce various chemokines, such as interleukin-5, that attract eosinophils and assist in killing infected cells (Kujime et al., 2000). The ERK pathway also induces the expression of transcription factors that are important for the induction of IFN. Chemokines and cytokines secreted by infected cells also attract monocytes and lymphocytes, such as neutrophils and macrophages, which phagocytose infected cells and also ingest cell-free virus in large numbers (Lemercier et al., 1979).
The epidemiologically important influenza A and B viruses are negative-stranded RNA viruses belonging to the family Orthomyxoviridae (Palese P, Shaw ML 2006). The genomes of these viruses are composed of 8 RNA segments, two of which code for immunologically important proteins, namely hemagglutinin (HA) and neuraminidase (NA). The HA and NA proteins are found on the surface of influenza viruses and are important for the recognition of these viruses by the immune system of infected hosts; such immunological recognition is the basis for the classification of influenza A viruses into subtypes. A total of 16 HA and 9 NA proteins with substantially distinct immunological recognition profiles have been identified among circulating influenza A viruses (Subbarao, K., Swayne, D.E., Olsen, C.W. 2006.). Only two H/N combinations, or subtypes, currently circulate in the human population – H1N1 and H3N2 — while viruses belonging to many other subtypes circulate predominantly among birds [2]. In contrast to type A influenza viruses, influenza B viruses are not divided into subtypes and they do not, in general, infect non-human hosts. Immunologically consequential point mutations to the HA and NA proteins give rise to antigenically “drifted” strains of influenza A and B viruses that are responsible for annual epidemics of influenza infection and related illnesses. These epidemics constitute an important cause of mortality, especially among young children, older individuals, and immunocompromised individuals World Health Organization (2003). Moreover, mutations to HA (and other viral proteins, in some cases) may give non-human-adapted influenza virus strains the ability to infect humans. Such a mutation-enabled “host-jump” occurred recently, when birdadapted strains belonging to the H5N1 influenza A subtype acquired the ability to infect humans, causing about 385 infections and 243 deaths World Health Organization (2008). There are concerns that strains of this subtype may eventually acquire the ability to spread efficiently among humans and, possibly, cause the next influenza pandemic Taubenberger JK, Morens DM, Fauci AS (2007). In addition to mutation, co-infection of the same host by different influenza virus strains may lead to the production of reassortant strains bearing segments derived from two or more of the infecting strains. Such reassortant strains could be relatively common Bean WJ, Cox NJ, Kendal AP (1980), Lindstrom SE, Cox NJ, Klimov A (2004), Holmes EC, Ghedin E, Miller N, Taylor J, Bao Y, et al. (2005), especially those carrying segments derived from different strains that belong to the same subtype. Of much greater epidemiological significance are human-adapted reassortant strains carrying HA segments obtained from non-human-adapted strains. During the past 100 years, such antigenically “shifted” strains were responsible for three influenza pandemics, the most devastating of which occurred in 1918.
To help address the threat of future influenza epidemics and pandemics the World Health Organization’s global influenza surveillance program was established 55 years ago and tasked with collecting data on the antigenic evolution of influenza viruses and using those data to forecast the emergence of epidemic and pandemic influenza viruses Cox NJ (2001), Layne SR (2006). The antigenic data used for these forecasts are obtained primarily by means of the hemagglutination-inhibition (HI) assay Webster R., Cox N, Stohr K (2002). The basic principles underlying the use of HI for influenza surveillance are the following Hirst GK (1941): (1) influenza viruses have the ability to agglutinate red blood cells, (2) antibodies can neutralize influenza viruses and, thereby, inhibit their red cell-agglutinating ability, and (3) the degree to which antibodies raised against one influenza virus strain neutralize the red cell-agglutinating capacity of another strain provides a measure of the antigenic similarity between the two virus strains (the main steps of the HI assay are illustrated in Figure 1 and are also described in greater detail in Theory and Methods). Presently, there is a paucity of reliable quantitative information about the biophysical determinants of HI data (i.e., HI titers). More specifically, there is inadequate knowledge about the manner in which both antigenically relevant and other underlying parameters contribute to HI titers. Such knowledge would not only allow comparisons of HI titers obtained under different experimental conditions (e.g., using different concentrations of virus and of red cell), it would also enable critical examination of existing approaches to interpreting HI titers.
While there are computational methods for inferring antigenic relationships from HI titers, Archetti I, Horsfall FL (1950), Smith DJ, Lapedes AS, de Jong JC, Bestebroer TM, Rimmelzwaan GF, et al. (2004), to our knowledge there has been only one serious attempt Lanni F, Lanni YT (1952), at shedding light on the nature of the biophysical interactions that determine HI titers. In particular, Lanni and Lanni investigated the kinetics of HI and derived mathematical equations for the dynamics of the concentration of, for example, virus-antibody and virus-red cell complexes. However, those authors did not derive an equation for the HI titer. Here, we investigate the kinetics of HI and derive a mathematical equation for the HI titer. Our analyses differ from those performed by Lanni and Lanni in important ways. Firstly, we use an equilibrium (as opposed to a non equilibrium) chemical kinetic framework that is motivated by previous experimental results. Secondly, we use a collision theory approach that allows us to account for virus-antibody and virus-red cell complexes of much more varied sizes than is practical with the absolute rate theory approach used by Lanni and Lanni. Thirdly, our emphasis is on shedding light on basic aspects of HI kinetics; therefore, we make a smaller number of simplifying assumptions about the nature of HI.
References
Antigenic and genetic characteristics of H5N1 viruses and candidate H5N1 vaccine viruses developed for potential use as pre-pandemic vaccines, WHO: August 18, 2006. http://www.who.int/csr/disease/avian_influenza/guidelines/recommendationvaccine.pdf
Beveridge, WIB. The chronicle of influenza epidemics. Historical and Philosophic Life Sciences 1991: 13, 223-235.
Breshsckin AM, Ahern, J, White DO. Antigenic determinants of influenza virus hemagglutinin. Virology. 1981; 113:130-140.
Bullough PA, Hughson FM, Skehel JJ, Wiley DC. Structure of influenza haemagglutinin at the pH of membrane fusion. Nature. 1994: 371, 37-43.
Centers for Disease Control and Prevention. Influenza 2005. Available from: URL: http://www.cdc.gov/ncidod/diseases/flu/fluinfo.htm.
Colman PM, Varghese JN, and Laver WG. Structure of the catalytic and antigenic sites in influenza virus neuraminidase. Nature. 1983: (303), 41-44.
Gerhard W, Yewdell J, Frankel ME. Antigenic structure of influenza virus haemagglutinin defined by hybridoma antibodies. Nature. 1981:290: 713-7.
Hay AJ, Gregory V, Douglas, AR, Lin YP. The evolution of human influenza viruses. Phil. Trans. R. Soc. Lond. 2001: 356, 1861-70.
Helenius A. Unpacking the incoming influenza virus. Cell. 1992; 69:577-578.
Helenius, A. Unpacking the incoming influenza virus. Cell. 1992: (69), 577-578.
Herrmann B, Larsson C, Zweygberg BW. Simultaneous detection and typing of influenza viruses A and B by a nested reverse transcription-PCR: comparison to virus isolation and antigen detection by immunofluorescence and optical immunoassay (FLU OIA). Journal of Clinical Microbiology. 2001: 39(1), 134-138.
Hirst, GK. The quantitative determination of influenza virus and antibodies by means of red cell agglutination. Journal of Experimental Biological Medical Science. 1942: (25), 227-233.
Hull, JD, Gilmore, R and Lamb RA. Integration of a small integral membrane protein, M2, of influenza virus into the endoplasmic reticulum: Analysis of the internal signal-anchor domain of a protein with an ectoplasmic NH2 terminus. Journal of Cellular Biology. 1988 (106), 1489-1498.
Kendal AP, Pereura MS, Skehel J. Concepts and procedures for laboratory based influenza surveillance. Geneva, Switzerland: World Health Organization, 1982.
Lamb RA, Choppin PE. The gene structure and replication of influenza viruses. Annual Review of Biochemistry. 1983: 52: 467-506.
Lamb, RA, Zebedee, SL, and Richardson CD. Influenza virus M2 is an integral membrane protein expressed on the infected-cell surface. Cell. 1985: (40), 627-633.
Li KS, Guan Y, Wang J, et al. Genesis of a highly pathogenic and potentially pandemic H5N1 avian influenza in eastern Asia. Nature. 2004; 430: 209-213.
Lin YP, Bennett, GM, and Hay, A. Recent changes among human influenza viruses. Virus Research. 2004: 103, 47-52.
Palese P, Compans RW. Inhibition of influenza virus replication in tissue culture by 2-deoxy-2,3-dehydro-N-trifluoro-acetly-neuraminic acid (FANA): Mechanism of action. Journal of General Virology. 1979: 33, 159-163.
Palese P. The genes of influenza virus. Cell. 1977; 10: 1-10.
Phipps LP, Essen SC, and Brown IH. Genetic subtyping of influenza A viruses using RT-PCR with a single set of primers based on conserved sequences within the HA2 coding region. Journal of Virological Methods. 2004: 122, 119-122.
Plotkin JB, Dushoff J. Condon bias and frequently-dependant selection on the hemagglutinin epitopes of influenza A virus. Proceedings of the National Academy of Sciences, USA. (2003); 100: 7152-7.
Portela A, Zurcher T, Nieto A, Ortin J. Replication of orthomyxoviruses. Advances in Virus Research 1999; 54: 319-238.
Potter, C.W. (1998) Chronicle of influenza pandemics. In: Textbook of Influenza. Nicholson, KG, Webster, RF, and Hay, AJ. Pp. 3-18. Oxford: Blackwell Science Ltd.
Qiu Y, Nemeroff M, Krug RM. The influenza virus NS1 protein binds to a specific region in human U6 snRNA andn inhibits U6-U2 and U6-U4 snRNA interactions during splicing. RNA 1995; 1: 304-316.
Reid AH, Fanning TG, Hultin JV, Taubenberger JK. Characterization of the 1918 “Spanish” influenza virus neuraminidase gene. Proc. Natl. Acad. Sci. USA 2000; 97: 6785-6790.
Reid AH, Fanning TG, Hultin JV, Taubenberger JK. Origin and evolution of the 1918 “Spanish” influenza virus hemagglutinin gene. Proc. Natl. Acad. Sci. USA 1999; 96:1651-1656.
Salk, JE. Simplified procedure for titrating hemagglutinating capacity of influenza virus and the corresponding antibody. Journal of Immunology. 1944: (49), 87-98.
Scheiffele P, Rietveld A, Wilk T, Simons K. Influenza viruses select ordered lipid domains during budding from the plasma membrane. Journal of Biological Chemistry. 1999; 274: 2038-2044.
Shimizu K, Iguchi A, Gomyou R, Ono Y. Influenza virus inhibits cleavage of the HSP70 premRNAs at the polyadenylation site. Virology. 1999; 254: 213-219.
Sieneke-Grober A, Vey M, Angliker H, Shaw E, Thomas G, Roberts C, Kenk HD, Garten W. Influenza virus hemagglutinin with multibasic cleavage site is activated by furin, a subtilisin-like endoproteaes. EMBO J. 1992: 11: 2407-2414.
Skehel JJ, Wiley DC. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annual Reviews Biochemistry. 2000; 69: 531-569.
Spackman, E, Senne, DA, Bulaga, LL, Myers TJ, Perdue, ML, Garber, LP, Lohman, K, Daum LT, and Suarez, DL. Development of a real-time reverse transcription PCR assay for type A influenza virus and the avian H5 and H7 hemagglutinin subtypes. Journal of Clinical Microbiology. 2002. 40(9), 3256-60.
Stockton J, Ellis JS, Saville M, Clewley JP, Zambon MC. Multiplex PCR for typing and subtyping influenza and respiratory syncytial viruses. Journal of Clinical Microbiology. 1998: 36, 2990-2995.
Watowich S, Skehel JJ, Wiley DC. Crystal structures of influenza virus hemagglutinin in complex with high-affinity receptor analogs. Structure. 1994: 2, 719-731.
Webster RG, Bean WJ, Gorman OT, Chambers TM, and Kawaoka, Y. Evolution and ecology of influenza A viruses. Microbiological Reviews. 1992: 56, 152-179.
Webster RG, Hinshaw VS, Laver WG. Selection and analysis of antigenic variants of the neuraminidase of N2 influenza virus with monoclonal antibodies. Virology. 1982: 117: 93-104.
Webster RG, Rott R. Influenza virus A pathogenicity: the pivotal role of hemagglutinin. Celll 1987; 50: 665-666.
Whittaker G, Bui M, Helenius A. The role of nuclear import and export in influenza virus infection. Trends Cell Biology. 1996 6: 67-71.
WHO changes H5N1 strains for pandemic vaccines, raising concern over virus evolution. CIDRAP (August 18, 2006). Available at: http://www.cidrap.umn.edu/cidrap/content/influenza/avianflu/news/aug1806vaccines.html
Wiley DC, Wilson IA, Skehel JJ. Structural identification of the antibody-binding sites of Hong Kong influenza haemagglutinin and their involvement in antigenic variation. Nature. 1981; 289: 373-8.
Yang Y, Halloran ME, Sugimoto JD, Longini IM. Detecting Human-to-Human Transmission of Avian Influenza A (H5N1). Emerging Infectious Diseases. 2007: 13(9), 1348-53.
Yuen KY, Chan Pk, Peiris M, et al. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet. 1998; 351: 467-471.
Zambon, MC. Epidemiology and pathogenesis of influenza. Journal of Antimicrobial Chemotherapy. 1999: 44, Topic B, 3-9.
Zebedee SL, Lamb RA. Influenza A Virus M2 Protein: Monoclonal Antibody Restriction of Virus Growth and Detection of M2 in Virions. Journal of Virology (1988): Volume 62 number 8: 2762-2772.
Zhang J, Leser GP, Pekosz A, Lamb RA. The cytoplasmic tails of the influenza virus spike glycoproteins are required for normal genome packaging. Virology. 2000; 269: 325-334.
Zou P, Liu, W, and Chen YH. The epitope recognized by a monoclonal antibody in influenza A virus protein is immunogenic and confers immune protection. International Immunopharmacology. 2005: (5) 631-635.
Need to buy a similar essay to ensure the best grades in your class? Fill the Order Form to send us the details of your requirements and get top class essay within the given deadline